Beyond “Empathy”: On being helpful
When you feel anxious, overwhelmed and uncertain about decisions related to your care, what characteristics do you seek in your doctor other than that “they know their stuff” (i.e. are clinically competent)? There has been a lot of talk over the years about the importance of empathy. The thought is that a distressed patient needs an empathic doctor. What is empathy, and why is it considered so important to clinical practice? I wonder whether the term draws too much attention to what the doctor is feeling and not enough to whether they are actually responding helpfully to whatever their patient needs.
Empathy has been defined as “an affective reaction caused by, and congruent with, another person’s inferred or forecasted emotions.” In the clinical setting empathy is described as “an experiential way of grasping another’s emotional states.” Because the term has a variety of meanings it is to difficult to assess whether it is an asset, but I’ve often felt the word is inadequate and perhaps misleading for capturing what a person who is in distress values and needs.
Speaking personally, the people I turn to in times of distress are those who will try to figure out what is going on with me to see if they can help. Some may feel empathy and others may not. If I recently had a heart attack I might be grappling with a foreboding sense of vulnerability and awareness of mortality. At the same time there could be practical concerns about my capacity to exercise, to have sex, to manage side effects of my medications and to reshape my self-image such that I am not pre-occupied with my health. If I hinted at these concerns, I’d want my physician to follow up with questions and then provide me with direction and reassurance if warranted.
That may all sound obvious, but our research indicates that most of the time doctors don’t do any of it. In one study we trained 8 actors to work as undercover patients carrying audio recorders, presenting to their doctors with relatively common clinical problems while, at the same time, dropping clues that they were facing serious challenges that were undermining their health or healthcare. In one case the “patient” presents with deteriorating asthma while taking an expensive brand name inhaler. He comments to his physician “boy, it’s been tough since I lost my job.” We saw three different responses: The largest group just ignored the comment. Busy typing their note, we’d hear something along the lines of “uh, huh….and do you have any allergies?” The second, relatively small number of physicians, acknowledged the comment along the lines of “I’m sorry to hear you are out of work. It’s been a rough economy lately.” The third, a minority, would inquire: “Can you tell me what you are struggling with?” Only to this group would the actors reply “I can’t afford my medication anymore so I’m taking it every other day.”
The first two groups got the care plan wrong every time because they never learned the real reason why the asthma was getting worse. They typically increased the dosage of a medication the patient already could not afford. Among the third group, doctors got the plan right about half the time. They’d switch the patient to a less costly generic. The other half, despite having learned the real reason their patient is clinically worse, still went up on the dosage of an unaffordable medicine. Although our actors dropped 4 hints at each encounter of a specific life challenge interfering with their care, physicians asked a follow up question and then addressed the concern just over 20% of the time.
What is going on here? Is the problem a lack of empathy? Are the 20% more empathic? I don’t think it is possible to answer such questions both because of the many ways the term is defined but also, more importantly, because one can never know what drives an individual’s behavior. What we can say is that the physician who notices signs of distress and asks about them, then tries to do whatever he/she can to help, is fundamentally caring. Her full attention is upon the patient. What she is feeling inside is unknown, perhaps even to her.
However one defines the term, to me at least, it puts too much emphasis on what the physician is feeling rather than on what they are doing to help the patient. The physician who feels empathy towards a patient who is struggling with their illness, but doesn’t find out whether there is something they can do to help is not helpful. Conversely, the physician who probes to learn that the patient can not longer afford his medication, is embarrassed to admit it, but would benefit from a generic may not feel anything in particular other than the satisfaction of being helpful. Which doctor would you prefer?
A colleague and I explored this topic in a paper titled From Empathy to Caring: Defining the Ideal Approach to a Healing Relationship. Part of the fun of writing that paper was that my co-author who I have observed to be one of the most caring individuals I know describes himself as entirely lacking in empathy. What he does acknowledge, however, is that he’d “stand on his head” during a visit if he thought it would help. That’s the kind of doctor I want.
Curious health providers also provide better care
There are two ways to learn what is really going on with another person who seems to be struggling: by asking them or by waiting for them to tell you. It turns out that when care providers are proactive and ask first, they are also more likely to help others cope with their challenges.
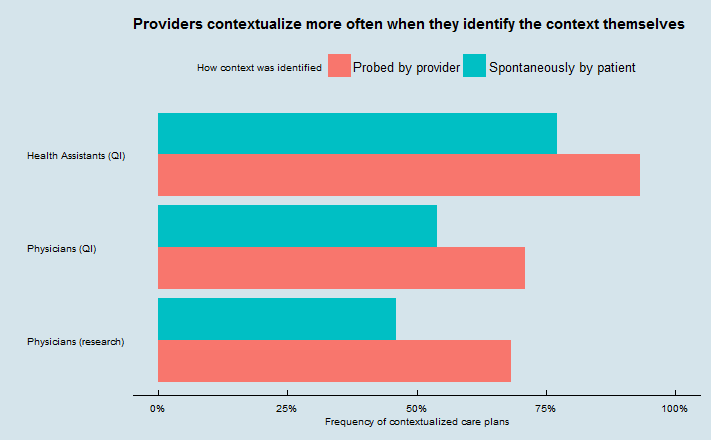
Our findings are in a new paper in a new paper in BMJ Quality & Safety. Specifically, we tracked how health assistants and physicians reacted to verbal cues that something in a patient’s life may be affecting their health care (what we call “contextual red flags.”) Providers who asked about these contextual red flags were more likely to act on what they learn than when their patient volunteers the information without being asked. For instance, if a patient has lost control of his diabetes (a contextual red flag) because he started working the night shift which has disrupted his diet, the physician is more likely to adapt the care plan if she learns about the life change by inquiring rather than having to be told.
How much more likely you ask?
 This is the kind of phenomenon that you can only discover by directly observing patient-provider interactions. We found this pattern by reviewing audiorecordings made during three different sets of encounters.
This is the kind of phenomenon that you can only discover by directly observing patient-provider interactions. We found this pattern by reviewing audiorecordings made during three different sets of encounters.
Two sets were recordings of visits between patients and physicians (209 visits from our research, and 1183 visits from a quality improvement project focused on improving contextualization), and one set was recordings of 96 telephone calls from clients to Accolade health assistants.
(Accolade is a novel company that contracts with employers or payers to provide telephone health assistants to aid employees/members with healthcare and claims needs. As you can also see from the chart, their health assistants do very well at contextualizing their advice – so much so that with their higher overall contextualization rate, 96 calls is not quite enough to call the difference in the chart significant using Accolade data alone. Full disclosure: our company, I3PI, consults for Accolade and had helped them study contextualization several months before we got the idea for this paper).
We found that value of physicians or other care providers actively asking patients about red flags that lead them to reveal relevant contextual information is not simply in the context that is revealed. The act of asking is associated with a greater chance that the context will actually be used to tailor plans of care. This could be because providers who are attuned to the importance of context do more asking and more tailoring than those who are not, or could be because asking and getting a positive response makes the context more salient (or both). Of course, it could also mean that providers only ask about context that they already know to how use.
Our take-home message: Providers should be encouraged both to ask more about potential context and to listen more when patients reveal it themselves.
Lecturing in the classroom produces lecturing in the exam room
If there is anything that requires critical thinking skills, it’s taking care of people who are ill. When someone is ill they have more than a disease. In fact, the clinician is presented with an individual whose homeostasis has been disrupted. Before you get sick, you have a routine and things are in some sort of balance: you go to school or work, find time to connect with friends and family, do chores, pay bills, take a shower, have sex, get rest etc…But when illness sets in, the precarious balance that is life before is perturbed. An effective clinician sees all this, and approaches the ill patient with a wide angle lens. He or she is able to discern what matters in a particular context. Our research on contextualizing care indicates that that ability is in short supply. A major culprit for such a profound competency deficit may be attributed substantially to a medical education process that still relies heavily on lecture.
First, a reminder, for those who have been out of school for a while….A colleague of mine with a lifetime of experience facilitating adult learning writes:
Lectures had been seen as the ultimate in efficiency – simultaneously force-feeding information into the ears of hundreds of students at a time as they were jammed into lecture halls with rows of fixed seating. Yet, in truth, the uncomfortable seats most often had too-small arms to support notebooks for the most inefficient mode of information transfer – from the mouth of the often mumbling professor, to the impaired ears of the students; set in a sea of noise from a hundred others scribbling, coughing, sneezing and shuffling impatiently; to the imperfect handwriting of a hundred ink-starved pens and broken-point pencils. This, for the past century and more, was the model of high-quality teaching (and learning). Forgetting the hearing-impaired, forgetting the sight impaired who could not read the black or white board, the lectures droned on.
Lecturing is basically telling people stuff while they are captive. It’s mostly unidirectional, and learners are rewarded for their regurgitating capacity. Once they’ve been through the system it becomes their turn to lecture to people. If they get PhDs they can lecture from a podium. If they get MDs they can lecture in the exam room. We hear doctors lecturing to patients about how they have to quit smoking, eat better, exercise more, take their pills…often using medical terminology, unaware that what they are saying is incomprehensible. What they don’t often do is ask their patient why they aren’t taking their pills or eating better etc…What does it say about a person’s critical thinking skills when they think they know how to fix something before they’ve looked into why it’s not working?
Lecturing at the lectern is equally illogical: The teacher is transmitting information without knowing the learning needs of a diverse audience. Some students, like patients, may benefit from the information transfer. But for most, there are other learning needs. I remember sitting in lectures in college on the French revolution and feeling like I walked in late even when I got there on time. I was lost from the beginning because I lacked a foundation of knowledge that the teacher assumed I had. Similarly, a clinician lectures a patient unaware of the underlying struggles that individual is facing. Most people who don’t take their medication as directed probably won’t benefit from a lecture on how important their medication is. What they need is someone who will ask them about their challenges integrating something new, scary and that often changes how they feel into their daily routines…and then help them find their own solutions.
Lecturing is disrespectful. Don’t get me wrong: some like it, which is just evidence of learned helplessness. Lecturing is based on the premise that I know what you need and I’ll do the talking. It is ego gratifying for the lecturer, as they have the attention of many others (or the appearance, thereof. Most are on Facebook). Most importantly, it puts the teacher and learner on an unequal plane. And that comes to model the relationship between doctor and patient.
Not all learning requires conversation. Rote memorization works best with flashcards. Comprehension comes from reading (lecture is an inefficient alternative with lower long term retention). But learning to solve complex problems — to analyze and evaluate information, and to formulate and test hypotheses (see Bloom Taxonomy) — that requires direct engagement with the material…and when the “material” is other people, it requires engagement with them.
As long as we continue to lecture medical students we are treating them the way we don’t want them to treat patients and we are denying them the opportunity to build the skills they need to provide effective care.
It really is the patient’s story
Attitude toward illness is one of the ten domains of context that we’ve documented in our work studying physicians’ skills at tailoring care to real patients’ needs. One thing that we often don’t appreciate is how important it can be for people to be able to explain their choices – not only to others, but also to themselves, in light of their past experiences and choices. We often experience our lives as unfolding stories, and we want those stories to make sense to us.
A recently published article in the journal Medical Decision Making looks at this (full disclosure: I am the editor-in-chief of that journal). In “My Lived Experiences Are More Important Than Your Probabilities: The Role of Individualized Risk Estimates for Decision Making About Participation in the Study of Tamoxifen and Raloxifene (STAR)“, Christine Holmberg and colleagues interviewed women who agreed or declined to participate in a trial of tamoxifen and raloxifene, medications that are used to reduce the risk of breast cancer but have potential side effects. These drugs appear to be underused, based on statistical evidence about the number of women who would, on the whole, benefit from them.
When they asked women about their decisions to join or decline the trial, they found that personal or family experiences with breast cancer and general concerns about the effects of taking medication were more important than information about the probability of breast cancer or side effects. The authors refer to this as “a decision-making process for or against STAR participation that was guided by personal experiences, attitudes, and beliefs.” Those who joined the trial and those who didn’t came to different decisions, but did so through similar considerations about their individual life context.
This work is in the tradition of decision psychology research by Nancy Pennington and Reid Hastie in what’s been called “explanation-based decision making” or the “story model”. Most often studied in jurors or consumers, the idea is that sometimes what seems to be important to people in their decision making is that they be able to explain their decisions – not only to others, but also to themselves. People want to place their choices in the context of their identity and lived experience, which is itself shaped by their past choices.
Combine these theories with work on “illness narratives” pioneered by Arthur Kleinman, and research on identity in health psychology, and the message is clear: no matter how “right” a choice may be on the evidence, it’s very hard for people to do it if it contradicts their personal story.
Physicians looking to engage with their patients need to be listening for these stories too.
Third year medical student: Imposter or Caring Advocate?
A recent column titled 10 thoughts on the transition to a third-year med student provides excellent advice for those entering this stage of their training, including insights from those finishing that year. Several mentioned coping with the imposter syndrome, the feeling that you are masquerading as something you are not. I would like to make the case here that the student who simply attempts to understand and help meet their patient’s needs without trying to be anyone other than who they are, need not fear they are an imposter.
When students occasionally mention to me that they feel like an imposter I pose this question to them: What do you think your patients are looking for when you enter the room that you have to fake? Often I hear responses such as “they expect me to know a lot” or “when I am asking them highly personal questions, they think they are talking to a real doctor who can help them.” Such responses suggest the student has an ideal in their head of what a real doctor is like. That ideal is characterized by expert knowledge and the confidence that is assumed to come from mastery of a field. Until you get there you are an imposter, the logic would have it….
I share with students my impression which is that what patients are looking for most when anyone enters their room is respect. Respect is not the same as politeness, although politeness is an essential component. When we respect someone we take them seriously. And when we take them seriously we relate to them as ourselves, not in a role of any sort. You never have to worry about being an imposter when you recognize that drawing on who you are may bring comfort to those you are serving.
Learning to integrate the persona of physician with preexisting self is a challenge for medical students and, all too often, I see a failure of integration. Many doctors seem to relate to patients as if they always have latex gloves on. There is a barrier there even when it isn’t necessary. Patients become some sort of breed, somehow apart from ordinary people and certainly not the same as “us.” This perspective of self versus other in the identity formation of the physician must be avoided at all costs. Avoidance comes from recognizing our shared humanity. As a wise colleague, Simon Auster, puts it: never forget that you defecate, urinate and fornicate just as your patients do (except he sometimes uses more colorful words).
It took me years out of residency to recognize that when I enter an exam room I’m just one person coming to see if I can help another. I am aware, of course, that the reason the patient came to see me the doctor is because I have special skills acquired through medical training. The extent to which I will need those skills or how best they may serve the patient remains to be determined at the start of each visit. If I really want to help that person I have to find out what is going on with them as it relates to their health. As a researcher, I’ve learned that physicians who do this effectively do not on average have longer visits. That’s because they figure out what the patients really needs early in the encounter.
I encourage medical students to offer patients much more than their neophyte clinical knowledge because they have much more to offer that patients need. I suggest that when they ask patients how they are doing, ask with the intention of really finding out how they are doing. If the patient has a chronic condition such as diabetes or hypertension, that is not well controlled, try to really figure out why. Don’t assume they just need a higher dosage of a medication or a reminder that they need to do a better job taking their meds. Chronic illness is a life challenge that comes with fears, competing priorities, costs and opportunities for personal growth. How are these impacting a patient’s health and health care?
Uncovering and then addressing these factors is what we mean by “contextualizing care.” The skills doctors need to do this well are not necessarily acquired through years of clinical practice. Unfortunately clinicians can spend decades practicing medicine without acquiring them, no matter how many facts they know and procedures they’ve mastered. On the flip side some people enter medical school having already acquired them. Such individuals are curious about what makes people tick, and know what questions to ask to pursue their curiosity. They also like to be helpful, finding satisfaction when they improve a situation. Many of us are somewhere in between. We are capable of regarding others through a wide lens, but after a few years in the medical education mill our perspective has narrowed: we are practically looking through a pinhole, both in terms of how we see our patients and how we regard ourselves.
So, if I were to propose an 11th piece of advice to third years it would be this: Rather than worrying about who you are trying to become, appreciate who you are and, in so doing, appreciate the person you are there to help.
The Doctor-Computer Relationship
In reflecting on a recent hospital stay, Alan Spiro observes “For those of you worried about depersonalization of medical and nursing care I want to reassure you. The commitment to caring for the computer is front and center.” He goes on to say “The nurse and the doctor are diligent in paying attention to the computer, frequently touching the computer to show concern, and feeding it frequently.”
While Dr. Spiro employs gentle irony and humor to make his point, the problem is serious and vast. My colleague Alan Schwartz and I have spent over a decade listening to doctors talk to patients during the medical encounter. In one study we employed actors as unannounced standardized patients (USPs) to conduct 400 visits to physicians who thought, at the time of the encounter, that they were seeing a real patient. In another, over 600 real patients carried concealed recorders into their visits for our analysis. More recently we’ve invited Veterans to carry concealed audio recorders into their appointments, so that we can collect data on missed opportunities to provide optimal care, and then feed that information back to participating doctors. Our team has listened to over a thousand of those. Often it’s painful to hear how the demands of the computer consume a visit.
Nearly everyone — including clerks, nurses and pharmacists (and we collect audio recordings of all of them) — is meeting a data entry expectation. For physicians in the outpatient setting it’s typically E&M coding. How distracted and preoccupied are providers? One of the things we do when we send in USPs is we instruct them to drop little bombs during the visit that should get any conscious clinician’s attention. For instance, a patient with diabetes who comes in with repeated episodes of near fainting, says “you know doctor, sometimes I take 12 of the long acting insulin and 24 of the short acting one and sometimes I think I do it the other way around. It all probably evens out.” In the best case scenario, the physician looks up from the keyboard and says something like “That sounds like a problem. Can you tell me more about the challenges you are having taking your medications as directed?” Such a response is rare. More often, the physician’s focus is on what to put in the EHR when their patient can’t feed them the data they need. We’ll hear: “So, it’s probably 24 of the long acting and 12 of the short acting. Right? That’s the usual way it’s prescribed. That’s what I’ll put here…” The significance of the patient’s confusion as a problem that needs to be addressed directly gets lost.
Remarkably, quite a few physicians do an impressive job of multi-tasking. They attempt to simultaneously follow the patient’s lead, while interjecting questions to meet the documentation requirements for billing purposes. So, while trying to follow up on a comment by a patient that “boy, it’s been tough since I lost my job” they are running through a mindless checklist about possible headaches, constipation, itchiness etc… But even these doctors often make a Faustian bargain: while they take a rational approach to conducting a physical exam, they chart things they didn’t do. Most typically, they record a normal “review of systems” and head-to-toe physical exam without completing either. Interestingly, this phenomenon, which has been called “the ethical problem of false positives” (others just call it fraud), pre-dates widespread use of the EHR. What that 2002 USP study on false positives does not pre-date is Evaluation and Management Coding, established by Congress in 1995 as a pre-requisite to bill for reimbursement.
The admonition that “if you didn’t document it, you didn’t do it” profoundly changed healthcare over a 20 year period. Doctors and nurses, and other providers, are judged based on the thoroughness of their record keeping. So much is riding on it: First, there’s billing. If you didn’t document enough, you can’t bill at a particular expected level. Second, if you didn’t document it, you could get sued and lose in court. And third, documentation is regarded as a measure of quality during peer review. Health care providers are frequently nagged about documentation issues. It can define their worth.
It’s human nature that if you are judged on something (and your paycheck is riding on it) you are going to make that your focus. So the focus of health care is making the medical record look terrific or, at least, complete. It doesn’t look terrific a lot of the time because of all the copying and pasting, and a lot of what’s in it turns out to be fabricated….but it certainly looks like everyone’s keeping busy.
What if we assessed care delivery based on actually observing it now and then? Our work, and that of others who employ unannounced SPs, suggests it is readily feasible and is eye opening. It provides a window into the challenges providers face, the trade-offs they make, and consequences both for care delivery and documentation of care delivery. In fact, if we started observing care directly (think mystery shopper program, but with rigorous standardization) we could liberate health care professionals to just do the right thing (aware that some of their patients are collecting data on their performance), document what’s clinically important, and direct their attention to the patient before them.
